
Every morning before dawn, Dhanam, a small business owner in Chennai, prepares her idli stall for the day. Fatigue was her constant companion till a free checkup by the Smile on Wheels mobile medical unit revealed that she had diabetes. With access to timely guidance and care delivered close to home, she has been able to manage both her health and her livelihood without missing a single customer in a day.
While India’s urban medical infrastructure has emerged as a global benchmark attracting international patients with its world-class hospitals and advanced treatments, the same cannot be said for rural healthcare. But this sheen of excellence fades quickly as one moves beyond city limits. In rural and underserved areas, healthcare is often an afterthought which remains delayed, distant, and fragmented.
The issue is not only the absence of hospitals or beds, but the critical shortage of skilled and often overlooked, shortage of skilled healthcare workers. Hospitals and clinics can be built, but without trained professionals to staff them, they remain symbols of intent rather than engines of impact.
A healthcare system without trained caregivers is a system destined to fail. For business leaders, CSR professionals, and policymakers, this challenge also presents an opportunity. Investing in rural health is a strategic investment in the nation’s social and economic infrastructure. Strengthening the rural health workforce fuels productivity, resilience, and long-term development goals. It ensures that no life remains unreachable, and that India’s rural healthcare transformation is truly inclusive.
Rural Healthcare Workforce Deficit
In India where healthcare professionals are often revered as “gods,” the expansion of modern hospitals, rising numbers of medical graduates, and a growing private sector have created an impression that quality healthcare is now within reach for all. Yet this perception masks the troubling truth that in countless remote villages across India, even a basic medical consultation remains out of reach. The closest doctor may be hours away, and trained nurses are often absent from the local primary health centre.
India’s rural healthcare system continues to fight the crisis of the acute shortage of trained human resources. Despite sustained government efforts and targeted interventions, the lack of doctors, nurses, and frontline workers in rural India remains one of the most critical barriers to delivering equitable care. Several interlocking factors explain why rural India remains on the wrong side of this imbalance.
- Geographical maldistribution and urban preference
Despite an overall increase in medical graduates over the year, recent surveys suggest that India has approximately 1:1456 of doctor-population ratio contradicting the WHO standards of 1:1000. A key challenge lies in the urban concentration of medical professionals. Increasingly, doctors are opting for city-based careers, drawn by better professional opportunities, higher earning potential in the private sector, and superior living conditions. This growing urban preference has contributed to the persistent difficulty in staffing rural healthcare facilities leaving large swathes of India underserved and vulnerable.
- Unsupportive rural working conditions
Persistent gaps in infrastructure such as unreliable electricity, limited access to clean water, inadequate staff housing, and non-functional diagnostic tools continue to plague rural healthcare systems in India. For doctors and medical personnel posted in remote areas, the lack of quality schooling for their children and the absence of secure, livable environments for both work and residence present additional barriers. These challenges collectively discourage healthcare workers from accepting or continuing rural postings, reinforcing the urban-rural divide in access to essential health services.
- Urban-centric medical education system
Medical and nursing education in India remains largely centred around tertiary care, with limited emphasis on preparing professionals for the realities of rural practice. This urban-centric training leaves graduates ill-equipped and often unwilling to serve in underserved regions. Compounding the issue is the stark mismatch between the number of MBBS graduates and the availability of postgraduate seats, pushing many aspiring doctors to forego rural postings in pursuit of further academic opportunities—a trade-off that continues to weaken frontline care in rural India.
- Systemic delays and administrative inefficiencies
Recruitment to India’s rural healthcare centres is often hindered by delayed processes, lack of transparent vacancy notifications, and bureaucratic red tape. These systemic inefficiencies not only slow down staffing but also deter many young medical professionals from applying to Primary Health Centres (PHCs) and Community Health Centres (CHCs), further deepening the rural health workforce crisis.
According to recent surveys, 65% of India’s total population lives in rural areas. Given this demographic reality, it is imperative to assess whether the country’s healthcare workforce aligns with the needs of its rural citizens.
Alarming data from the National Medical Journal of India indicates a shortfall of nearly 80% in rural healthcare staffing, even as infrastructure has expanded. Since 2005, India has witnessed a 63.8% increase in the number of Community Health Centres (CHCs). As of 2022, there were 5,480 CHCs operational in rural areas, supplemented by 584 in urban settings. In tribal regions, 960 CHCs have been established, signalling a concerted effort to reach historically underserved populations.
Notably, states such as Uttar Pradesh, Tamil Nadu, West Bengal, and Bihar have led the way in expanding healthcare infrastructure, reflecting targeted efforts to mitigate regional health disparities. However, infrastructure alone cannot deliver care without adequately trained and retained personnel, these centres risk becoming underutilised assets.
Public Health Chronicles*
Government initiative for healthcare in India
In alignment with Sustainable Development Goal 3 and India’s health priorities, the government is working to build a more inclusive and resilient healthcare system, especially in underserved regions. Recent reforms focus on strengthening frontline infrastructure, expanding workforce capacity, and leveraging digital solutions to close critical service gaps.
- Ayushman Bharat – Health and Wellness Centres (HWCs):
These centres provide comprehensive primary care including maternal and child services, NCD screenings, and essential medicines bringing preventive and promotive healthcare closer to rural communities.
- National Health Mission (NHM):
Launched in 2013, NHM integrates rural and urban health missions, emphasizing decentralized planning, community engagement, and system-wide improvements.
- Human Resource Reforms:
Using Rural Health Statistics to guide decisions, policy measures now target recruitment bottlenecks, workforce incentives, and training reforms to ensure skilled personnel reach India’s remotest health centres.
Human resources for health – The critical pillar of Indian rural healthcare
The World Health Organization defines the Human Resources for Health (HRH) as all individuals engaged in promoting, protecting or improving public health. It includes clinical care, public health interventions, research, management and support services. (WHO,2007). Their role and capacity directly influences health outcomes and system efficiency.
When there is a low HRH density, its direct impact is seen in increased maternal and child mortality, reduced life expectancy, and a growing burden of untreated mental health conditions. The shortage of healthcare givers in the rural landscape of India also becomes a concerning factor towards implementation of health policies to its full effect, disrupting continuity of care, and posing a significant barrier to achieving public health goals. Most critically, it threatens the country’s progress toward Universal Health Coverage.
What’s needed? A people-first approach
Like any profession, healthcare demands a robust, supportive ecosystem. One that nurtures not only clinical expertise but also professional development, career advancement, and personal well-being, especially in high-demand, resource-limited settings like rural India.
To address this systemic gap, health policy experts and medical academicians have put forward strategic recommendations aimed at bridging the divide between trained healthcare providers and the underserved rural population. These include:
- Providing the medical personnels with rural healthcare fellowships programmes
- Provide them with incentivised service models like housing, pay structure, and career recognitions
- Strengthening community-based solutions by promoting the training of local women as ASHA workers and auxiliary nurse midwives
- Digital upskilling and telemedicine integration
These interventions recognise that rural health systems must be built from the ground up and not imposed from the top down. By encouraging local leadership, creating enabling conditions for healthcare professionals, and aligning incentives with service delivery, India can create solid, sustainable pathways for its rural health workforce.
Partnerships that strengthen people power
In the remote interiors of Tamil Nadu, a community of daily-wage labourers survives on earnings that barely cover basic necessities. For them, healthcare was a luxury, an added financial strain they simply cannot afford.
However, that narrative has begun to shift. Through a strategic partnership with a leading multinational health technology firm, Smile Foundation’s Smile on Wheels mobile medical unit now brings accessible, no-cost primary healthcare directly to their doorsteps.
Regular check-ups, preventive screenings, and free medicines have empowered pregnant women, children, and the elderly to take charge of their health without the anxiety of added financial burden.
This model demonstrates how targeted CSR partnerships can bridge systemic healthcare gaps, enabling low-resource populations to live healthier lives sustainably and with dignity.
Corporate Social Responsibility towards building a robust healthcare system is not a new phenomenon but definitely one of the most powerful tools to strengthen it. Since ages, corporate partnerships for healthcare have played a pivotal role in advancing the healthcare goals of the country bringing quality healthcare services and dignified lives to the underserved communities of India.
Therefore, their role in solving the challenge of limited healthcare givers in India is more important to support and implement the initiatives taken by the state for a healthier India.
- Support training of frontline workers in India’s rural healthcare system
Training the rural healthcare workers strengthens community-based care, improves health outcomes and builds trust in the system. By investing time and efforts, corporate partnerships can empower women and children with better healthcare facilities, enhance workforce retention, and ensure sustained impact leading to compassion meeting the true potential of the frontline workforce in delivering quality healthcare.
- Invest in technology enabled capacity building
Technology driven solutions such as e-learning platforms, mobile medical units, and telehealth services extend the reach of quality care. These tools bridge access gaps, enable real time diagnostics, and foster last mile impact- transforming healthcare delivery for underserved communities while ensuring cost efficiency and positive impacts.
- Partnering with NGOs in India to develop and deploy rural health talent pools
By partnering with trusted development organisations in India, corporates can enable scale deployment of trained health professionals in rural regions. These collaborations create sustainable talent pipelines, rooted in local context, ensuring continuity of care, community trust, and measurable healthy system strengthening at the base level.

Achieve Universal Health Coverage goals with Smile
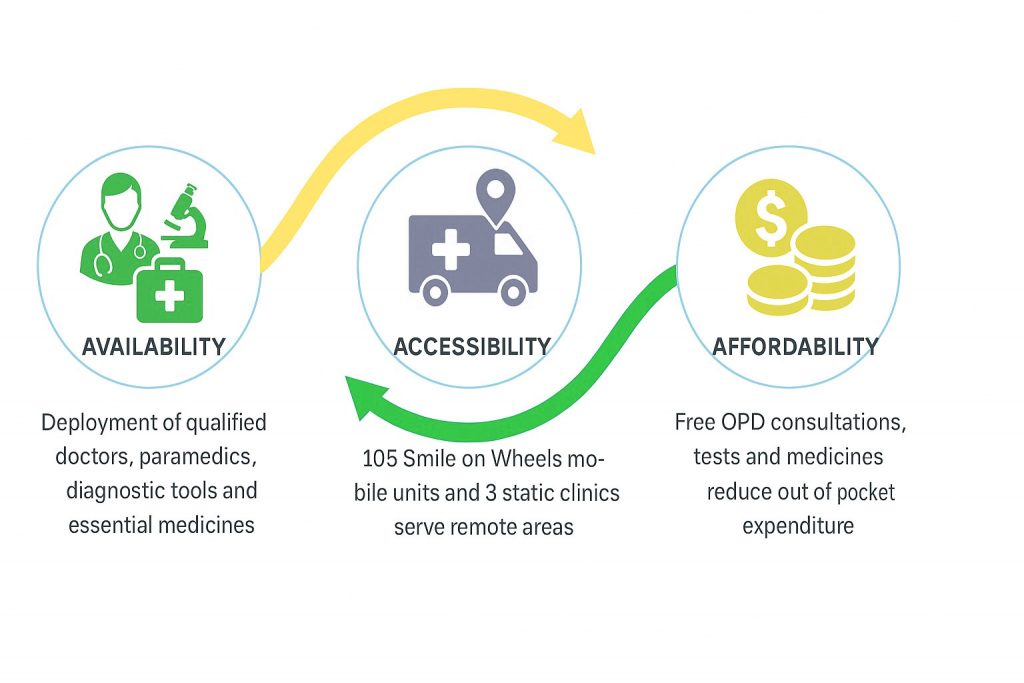
Smile Foundation’s healthcare programme reaches over 12.89 lakh people across 16 states directly contributing to SDG of ensuring health and well being for all. The initiative delivers primary healthcare at the doorstep for the underserved communities of the country where the focus on 3A’s – Awareness, Affordability, and Access are delivered at the doorstep.
With the goal of building capacity and promoting changed behaviour, Smile’s healthcare interventions in 2024 have conducted 23 nationwide training for frontline healthcare workers combined with targeted IEC campaigns, promoting long term health seeking behaviours addressing antenatal care to diabetes, hygiene, and geriatric support.
To advance last-mile healthcare solutions, the programme has also introduced mobile dental clinics and established Transport Aarogyam Kendras for truck drivers who often forgo medical care due to cost or limited access. These efforts aim to bring quality healthcare directly to populations typically left on the margins.
At Smile Foundation, we see our grassroots health programmes as a clear opportunity for companies to meet their CSR goals. Partnering with us means delivering inclusive, technology-enabled, and community-centric healthcare to rural communities where the need is urgent and the impact is lasting.





