Over 65% of India’s population lives in rural areas, but healthcare infrastructure and personnel remain disproportionately urban-centric. Punjab’s rural communities, home to ~17.9 million people, face a 20% shortfall in health sub-centres, fewer Primary Health Centres (PHCs) than needed, and a huge gap in Community Health Centres (CHCs). As a result, each rural sub-centre in Punjab serves on average 6,258 people (vs the national norm of 5,000) and each PHC covers 45,000 people (vs norm 30,000). These shortages are compounded by severe workforce gaps – for instance, rural CHCs in Punjab have only 55 specialist doctors against 336 required (over 80% vacancy).
Many facilities also lack basics like electricity and water: in 2023, 299 of Punjab’s 2,857 rural sub-centres had no electric supply and dozens lacked running water. This infrastructure deficit undermines service quality and deters healthcare utilisation, especially among vulnerable groups (women, children, the elderly). It reflects a broader inequity.
Globally, 56% of people in rural areas do not have access to essential health services, contributing to worse health outcomes and avoidable mortality. Bridging these gaps in accessibility is crucial for India’s commitment to Universal Health Coverage (UHC) and health equity.
Telemedicine has emerged as an effective solution to the rural healthcare crisis, by breaking geographical barriers and bringing medical expertise virtually to underserved areas. India’s national telemedicine platform eSanjeevani exemplifies this potential – since launching in 2019, it has facilitated over 34 crore (340 million) consultations as of Feb 2025, connecting remote patients with doctors and specialists.
During the COVID-19 pandemic, telemedicine proved indispensable in maintaining care continuity in remote regions. The Government’s two-pronged eSanjeevani system – AB-HWC (Ayushman Bharat-Health and Wellness Centre) for provider-to-provider consultations via Community Health Officers (CHOs) at rural clinics, and OPD for direct patient-to-doctor online visits – has helped ensure availability, accessibility and affordability of healthcare across India. However, leveraging telehealth at scale also requires robust digital infrastructure, training, and community trust. Studies indicate that without adequate training and protocols, telemedicine referrals can be sub-optimal, and limited digital literacy or connectivity in rural areas remains a barrier. Addressing these challenges is essential to realise telemedicine’s full impact.
Punjab, with relatively high mobile penetration and improving broadband reach, is well-positioned to benefit from telehealth innovations – provided the rural clinics are upgraded with power supply, internet, and skilled staff. This is the context in which Smile Foundation’s telemedicine initiative in Moga district, Punjab, was conceived as a public-private partnership model to strengthen rural primary care delivery.
Smile Foundation telemedicine initiative in Moga, Punjab
Moga, Punjab – identified under India’s Aspirational Blocks Programme for its lagging health indicators became the focus of a telemedicine-led healthcare strengthening project in 2023-24. Smile Foundation, in collaboration with the Health Department of Punjab, and corporate partner SBI Cards, launched a comprehensive telemedicine initiative to bolster primary healthcare in Moga’s rural blocks. This model builds on Smile Foundation’s prior success in Nuh (Haryana), adapting it to local needs in Punjab.
The project’s core intervention is the establishment of 12 e-Arogya Telemedicine Clinics at government Health and Wellness Centres (sub-centres) across Moga. Each clinic is equipped with a telemedicine kiosk, digital diagnostics (point-of-care devices), and a Medicine Vending Machine (MVM) for instant dispensing of essential drugs prescribed during tele-consultations. Crucially, the project invested in infrastructure upgrades and identified sub-centres were refurbished along with outfitting of solar power units in them to ensure 24×7 electricity, and providing reliable internet connectivity to support uninterrupted tele-consultation sessions. This approach directly addressed the basic facility gaps, like electricity, that previously hindered digital health services in Punjab’s villages.

By December 2023, necessary government approvals were obtained and the telemedicine units were integrated with the national eSanjeevani platform, aligning the project with the Ministry of Health’s digital health ecosystem.
Capacity-building and community engagement
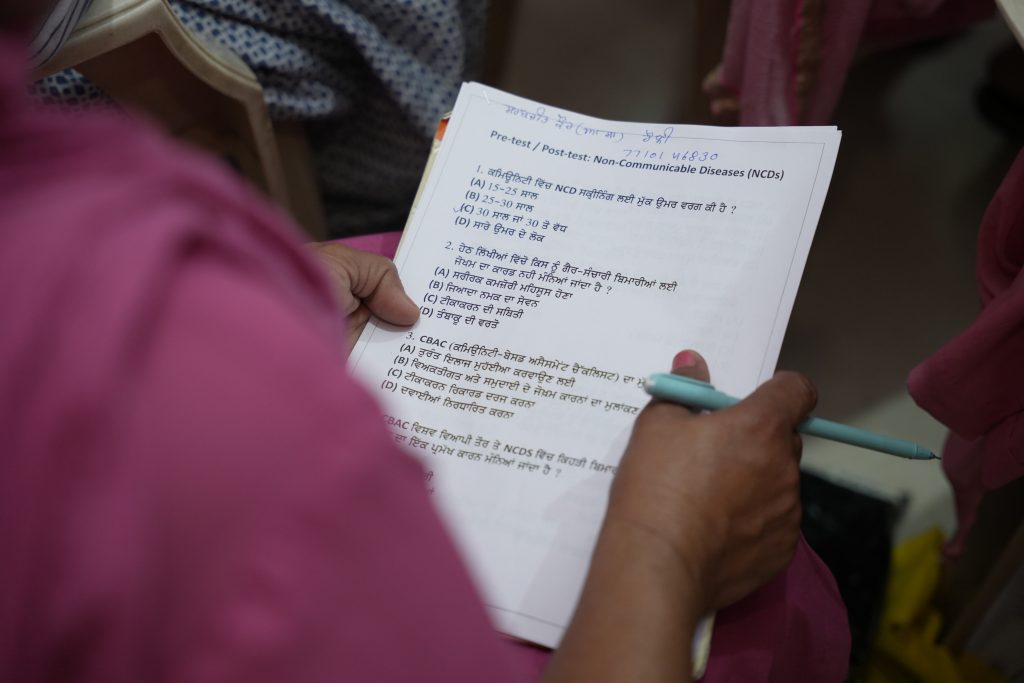
Capacity-building and community engagement form a major pillar of the Moga initiative. In partnership with state authorities, Smile Foundation conducted training for local healthcare providers and Frontline Workers. In late 2024, a two-day training for 180 frontline staff (CHOs, ANMs, ASHAs) from Moga’s health centres was held, focusing on management of common Non-Communicable Diseases (NCDs) like hypertension, diabetes, and screening for breast, cervical, and oral cancers. This skilling-up of workers aimed to ensure they can effectively use the telemedicine equipment, triage patients, and promote continuity of care.
“Strengthening healthcare at the grassroots” also involved behaviour change communication in the community – health awareness camps, village meetings, and mobilisation by ASHA workers to increase acceptance of teleconsultation services. The programme specifically targets women and marginalised groups for outreach, in line with Smile’s Swabhiman (women’s empowerment) programme. Notably, Dr. Neena Bansal, Senior Medical Officer in Moga, commended the initiative and presented a Certificate of Appreciation to Smile Foundation for its contribution to upgrading rural Health and Wellness Centres.

By early 2025, the e-Arogya clinics in Moga have begun offering remote consultations with MBBS doctors and specialists (located at hub hospitals) via eSanjeevani, free medication for patients through the MVM linked to government supply, and routine NCD risk-factor screenings – bringing primary care delivery that normally required travel to district hospitals directly to villages.
Improved primary care delivery and health access outcomes
Though the Moga telemedicine project is in its early stages, it draws from the proven impact of Smile Foundation’s earlier telehealth intervention in Nuh district, Haryana which offers a template for expected outcomes. Nuh, a predominantly rural and socio-economically challenged area (ranked among India’s Aspirational Districts), saw its first Smile telemedicine unit launched in May 2021. By mid-2023, this had expanded to 10 e-Arogya clinics across 8 PHC areas in Nuh, covering a population of about 10 lakh (1 million). The results have been remarkable in enhancing healthcare utilisation and equity.
In a one-year period (April 2022–March 2023), Nuh’s telemedicine centres facilitated 32,789 doctor consultations for villagers who otherwise face barriers to access. Importantly, over 53% of patients were repeat users (multiple visits), indicating high satisfaction and trust in the quality of care. The telemedicine clinics also integrated NCD screenings into their workflow, leading to thousands being screened for diabetes, hypertension, and other conditions per government protocols, with data reported into the public health system for follow-up. Such integration with the national NCD programme means earlier detection and referral of cases (e.g. identifying hypertensive patients who were unaware of their condition), reinforcing primary care’s gatekeeping role.
💬 Ask a CHO: Your Questions Answered
Gender-equity impact
Critically, the Nuh model demonstrated a gender-equity impact. Of the 35,000+ individuals directly benefitting from the telemedicine clinics in Nuh’s first two years, 52% were women – a notable achievement in a conservative region where women’s healthcare-seeking outside the home was very limited. Community women who “could not think of going outside the village” for care were now comfortably accessing medical consultations virtually in their local clinic. This reflects how telemedicine can overcome socio-cultural barriers by providing primary care delivery in a familiar setting. Patients received not only primary consultations but also referral support: the telehealth system in Nuh is linked with higher centres – about 2–3% of cases each quarter were referred to secondary/tertiary hospitals for issues needing in-person intervention, with the telemedicine staff facilitating these referrals. By managing the bulk of routine ailments and follow-ups at village level, the project helped decongest higher hospitals and cut down out-of-pocket expenditures (e.g. travel costs) for the community. Local health officials in Nuh noted a visible increase in outpatient footfall at the upgraded sub-centres due to telemedicine and NCD services, which in turn meant earlier treatment and better monitoring of chronic conditions.
Strengthening of the public health system
Another key outcome from Nuh has been the strengthening of the public health system through collaboration. The telemedicine units were eventually integrated into the government’s eSanjeevani network and handed over to the District Health Administration for sustainable operations. All 10 units in Nuh are now run as part of the Ayushman Bharat-Health and Wellness Centre scheme, with trained CHOs managing the teleconsultations – effectively institutionalising the innovation. This sustainability plan was built in by Smile Foundation from the start:
“We focus on setting up telemedicine clinics under a PPP model and later handing them over to the government to operate,”
noted Mr. Santanu Mishra, Co-Founder of Smile Foundation.
Indeed, the Nuh telemedicine project was recognised nationally, winning the ASSOCHAM “Best CSR Excellence in Healthcare” Award in 2023 for its impact in an aspirational district. Punjab’s Moga initiative is following the same trajectory. Initial indications show improved health awareness and service uptake in target villages of Moga. The project has set quarterly targets (e.g. ~4,300 teleconsultations per quarter by late 2024, scaling to ~10,000+ per quarter by late 2025), and will similarly be evaluated on reductions in patient travel, better management of NCDs, and patient satisfaction. Already, the collaborative training and enhanced infrastructure have prepared Moga’s health sub-centres to function as “model health and wellness centres”, offering a broader range of services than before.

Toward equitable and scalable primary care delivery models
The telemedicine model in Moga, and previously in Nuh, highlights how digital health can catalyse equitable healthcare delivery when combined with investments in primary care and community engagement. These interventions directly contribute to national health goals and international targets. By bringing doctors to the remotest communities virtually, such projects are “ensuring healthy lives and promoting well-being for all at all ages,” advancing Sustainable Development Goal 3 on health. They operationalise the Indian government’s vision under the National Health Policy 2017 and Ayushman Bharat: namely, leveraging digital technology to increase access, improve quality, and reduce the cost of healthcare delivery.
The Ayushman Bharat Digital Mission (ABDM) provides a supportive framework for interoperability and electronic health records, which the Moga telemedicine clinics are utilising to generate digital health records and share data on NCDs with state systems. Notably, Moga’s inclusion in the Aspirational Blocks Programme means it receives coordinated support to uplift health indicators – WHO India is one of the partners in this effort, focusing on primary health care strengthening and capacity building in Punjab’s aspirational blocks.
The power of public-private partnership (PPP) model
Smile Foundation initiative dovetails with this by addressing service delivery gaps on the ground. It demonstrates a scalable public-private partnership (PPP) model: the private sector (NGO and CSR funding) innovates and pilots the service, while the public sector provides facilities, integrates the services into its schemes, and sustains them long-term. Such models can be replicated in other under-served districts and blocks. Indeed, the Government of India is expanding telehealth through eSanjeevani to all 1.5 lakh Health and Wellness Centres nationally, learning from these pilots.
Digital infrastructure is now recognised as a critical determinant of health access. Moga’s project showed that investing in basics like power and internet connectivity for rural clinics is a pre-requisite to digital health solutions – a lesson for scalability. As rural broadband improves under programmes like BharatNet, telemedicine’s reach will further expand. However, human infrastructure is just as important: continuous training for health workers, digital literacy for patients, and trust-building in communities are vital for success. The Moga initiative’s use of local language educational materials and involving community leaders (Panchayats, village health committees) has been key to winning acceptance – villagers see the telemedicine clinic as an extension of the public health system, not a foreign technology. This community-centric approach aligns with WHO’s emphasis on people-centred primary care and reducing rural-urban health disparities. The World Economic Forum has lauded India’s digital health progress, noting that “telemedicine platforms are overcoming geographical barriers and reaching remote populations with quality care, thus bridging healthcare disparities.”
Reaching the last mile
In conclusion, Smile Foundation’s telemedicine initiative in Moga, Punjab exemplifies a data-driven, collaborative strategy to strengthen rural health systems. Early evidence and comparative insights from Nuh indicate that such interventions can substantially improve health system accessibility, by providing “last-mile” connectivity for medical services, enhance primary healthcare delivery through comprehensive services at the community level, and build digital health infrastructure that leaves a lasting impact. With supportive policy integration, these models contribute to a more equitable healthcare framework – one where a villager in Moga or Nuh can access timely, quality medical advice as readily as someone in a city.
As Punjab and India at large work towards universal health coverage, scaling up successful telemedicine-public health hybrids could very well be a game-changer for underserved regions. The Moga telemedicine project, supported by multi-sectoral partnerships and aligned with national programmes, is not only delivering care today but also providing a proof-of-concept for sustainable, tech-enabled primary healthcare that can be reproduced across India’s aspirational districts and beyond.
By addressing both the supply-side (infrastructure, providers) and demand-side (community awareness, affordability) barriers, it charts a path toward bridging the rural health divide and ensuring that geography is no longer destiny when it comes to primary care delivery access.
Sources: Punjab rural health statistics; Smile Foundation reports and press releases; WHO/WEF analyses; Government data on eSanjeevani. All data and insights are current as of 2024-2025, reflecting the latest available information on telemedicine interventions in India.
👣 Telemedicine Journey Simulator
Select a patient to begin their healthcare journey:
The journey will appear here once a persona is selected.










